Content
A big step forward: the AOSpine thoracolumbar spine injury classification system
For the past 6 years, the AOSpine Knowledge Forum Spinal Cord Injury & Trauma has been developing a new classification system for thoracolumbar (TL) injuries. This new TL system will be communicated to faculty this summer so they can teach it effectively. Cervical and sacral classification systems are next on the list.

Read an interview with spine surgeon Sallehuddin bin Abdullah from Malaysia, who was involved in the validation process.


The new AOSpine thoracolumbar spine injury classification system is based on the evaluation of 3 basic parameters:
1. Morphologic classification of the fracture
2. Neurologic injury
3. Clinical modifiers
There is no universally accepted spinal injury classification system, despite some attempts at developing one. AOSpine has used the Magerl concept since 1994, which was found to be rather complicated. The Magerl classification has not been clinically validated or revised to improve its reliability and clinical applicability.
In a quest to introduce simplicity and reproducibility to injury classification,the AOSpine Knowledge Forum Spinal Cord Injury & Trauma partnered with a number of surgeons. Together they have developed a systematic morphologic fracture classification and grading system for neurologic status and description of relevant modifiers for the thoracolumbar (TL) area. One key element of the development process has been rigorous scientific assessment. Development of cervical and sacral injury classification systems will begin in the near future.
Faculty involvement
The AOSpine TL Spine Injury Classification System was endorsed by the AOSpine International Board in December 2013. The AOSpine Education Commission will decide on the next steps and discuss how to implement the new classification system into AOSpine's education this spring.
Here we have a good example of how such a project progresses through the organization: previously the responsibility of the Research department in the development phase, the project is now now part of Education with the focus on determining the best way to train faculty in its use and incorporation into the AOSpine Curriculum.
Dr Luiz Vialle, former Chairman of AOSpine and one of the TL project leaders, is scheduled to conduct webinars on the TL system for course chairpersons. Attendance is mandatory and according to Dr Vialle this “will consolidate the classification as the AOSpine one.”
A clear cascade
A strength of the new TL system is that it is based on 3 morphological parameters so x-rays and CT scans should be sufficient to classify most injuries making fewer expensive MRIs necessary. Other classification systems consider ligaments, which are only visible with MRI imaging.
"The new system is based on the old Magerl one but we have aimed for simplicity—now there are only 9 sub-classifications for TL, not 25. The goal was to make it a concise tool that people could actually use,” said Patrick Hiltpold, AOSpine International Research Project Manager.
While the new framework is similar to the Magerl system, a simple algorithm has been generated to guide surgeons through a clear "cascade" of 3 main fracture types and 9 sub-types:
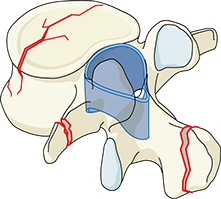
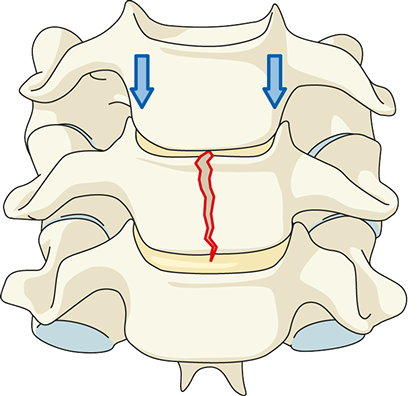
• Type A: Compression injuries—Failure of anterior structures under compression
• Type B: Distraction—Failure of the posterior or anterior tension band
• Type C: Translation—Failure of all elements leading to dislocation or displacement
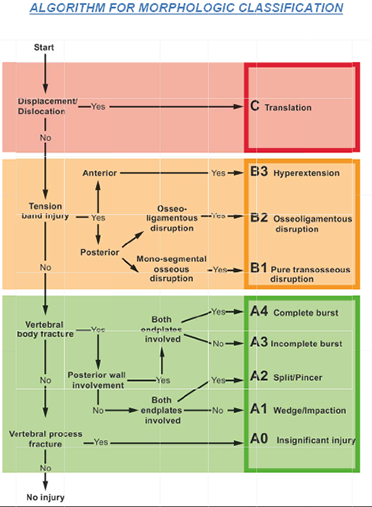
Algorithm for morphological classification
The classification process
An AOSpine working group (AOSpine Classification Group) has systematically assessed and revised the Magerl classification using an AOSpine database of more than 750 spinal trauma cases with DICOM images in order to develop a rational, simple, and reproducible morphologic classification. This working group conducted evaluation sessions to assess the reliability and accuracy and identified areas of disagreement requiring further refinement until a consensus was reached regarding classification details and application of the system, and adequate reliability was achieved. 7 face-to-face meetings and 5 evaluation sessions were ultimately necessary to achieve a consensus system for grading TL fracture morphology.
Neurological status and modifiers
6 neurological grades, as assessed upon admission, have also been provided and for a complete assessment, should be considered in combination with the 2 modifiers.
Neurologic assessment scores
• N0: Neurologically intact
• N1: Transient neurologic deficit, which is no longer present
• N2: Radicular symptoms
• N3: Incomplete spinal cord injury or any degree of cauda equina injury
• N4: Complete spinal cord injury
• NX: Neurologic status is unknown due to sedation or head injury
Modifier M1 provides flexibility in designating fractures with an indeterminate injury to the tension band. Modifier M2 lets surgeons designate patient-specific comorbidities that may influence surgical indications, such as ankylosing spondylitis or burns affecting the skin overlying the injured spine.
Proof is in the process
This sizeable task was accomplished using a structured consensus process of successive development and evaluation sessions building upon each other. For 6 years the Knowledge Forum Spinal Cord Injury & Trauma and AOSpine Classification Group have worked together on this project.
Members of both groups met numerous times, systematically discussing existing classification systems, refining the Magerl system, assessing reliability and accuracy, and identifying areas of disagreement that had to be refined until an unanimous consensus was reached on both classification details and application.
They accessed the AOSpine database of over 750 spinal trauma cases with DICOM images. 7 face-to-face meetings and 5 evaluation sessions were ultimately necessary to achieve a consensus system for grading TL fracture morphology.
Validating the system
Involving experienced surgeons from the AOSpine network has been integral to validating the new TL classification system. Now the framework has been set, a standardized testing of the system is underway. This testing is two-fold.
First, thirty selected cases have been provided to the working group to individually classify them according to the new system, then again in a randomized manner to see if results are reproducible.
The second step in validation involves 100 surgeons from around the world classifying cases to see if results are reproducible on a large scale and over cultural divides.
On the horizon
The next systems to be revised will also involve the same scientific process as it has proved to be quite robust. The subaxial cervical classification system will be available next and the sacral classification process will begin in 2015.

"The current utilization of this classification is not for the purpose of publication only but mainly of the training process with more than 100 surgeons around the world, surpassing economic and cultural influences. This is making the difference right now. In summary it was not only the delivery of a useful classification but the teaching methods and the involvement of the education commission which are an important success factor.”
Dr Luiz Vialle,
Former Chairman of AOSpine and associate member of the Knowledge Forum Trauma.

TL Classification system: validating regional interpretations
Sallehuddin bin Abdullah, a spine surgeon in Malaysia, shared some of the insights he gained as one of the team of surgeons involved in the validation process.
How did you become involved in this study?
I was asked to evaluate the new TL classification system. After a brief online training session in May 2013, I was given two assessments to validate. I am one of 100 surgeons who participated in this stage of the project.
What is your personal opinion of the new TL classification system?
I have used the previous classification system in my practice for over five years. Now that I have been able to also incorporate the results of this study, I have found the question of stability to be much more clearly defined. The obvious algorithm for morphology and the ABC classification is very good in terms of designating anterior or posterior tension band involvement. Incorporating the neurologic and the M1 and M2 modifiers is important I think. Being able to account for co-morbidities is very valuable.
What regional differences have you encountered in the practice of spine surgery that would impact the use of this classification system?
The issue of regional differences is very real and interesting. I have been trained in a number of countries and depending on where you are, there are different primary considerations when treating a spine injury. Firstly, cost limitations vary greatly according to where you are operating. Not all regions have health insurance coverage. Secondly, availability of implants impacts treatment as some are just not available in certain places. Thirdly, patient considerations vary. In Germany, for example, a patient wants to be operated on. In South Africa, they do not want operations unless they are absolutely necessary. Finally, the skill level of the surgeon plays a role. Not many surgeons are comfortable with an anterior approach to the spine but AO is changing this with its training and exposure around the world.
AOSpine
www.aospine.org | education@aospine.org
Copyright © 2014 AO Foundation. All rights reserved.

