Robots in Spine Surgery and Interview with Dr Kornelis Poelstra
Global Spine Focus
AOSpine Past Fellows are gathering at Global Spine Congress 2017
AOSpine Member Representative – Presentation of shortlisted applicants
AOSpine Members-only sessions at the Global Spine Congress
AOSpine Europe and Middle East

Share this article
00:00
00:00
Elon Musk is currently giving us taste of what advanced technology can do with Teslas that have all the hardware needed for full self-driving capability at a safety level substantially greater than that of a human driver. Is it likely that robots will have the same impact on spine surgery as advanced soft- and hardware technology will have on the automotive industry?
With spine surgery requiring steady hands for often long and arduous procedures, meticulous fine motor skills, as well as harmful radiation exposure, it is an ideal field for the integration of navigation and robotic-assisted procedures.
Whilst robotic systems have been used in many other surgical disciplines for a few years already, robot-assisted spinal surgery has only become available relatively recently. With the arrival of real-time image guidance and navigation capabilities, along with the software reliability and ability to process and reconstruct these data into an interactive three-dimensional spinal map within a blink of an eye, the applications of surgical robotic technology have taken a huge leap forward in the past 12 months.
But although this is an incredibly captivating area, many surgeons are still hesitant to use the technology for various reasons. Commercially available robots, however, are gaining acceptance by the community, indicating strongly that robotic-assisted surgery may become the standard of care in the future. Recent, carefully controlled studies have shown reduced complication rates-, re-admission rates-, and lower re-operation rates when robots were used compared to open- or ‘free-hand’ MIS spinal surgeries.
Goodbye to software crashes and lengthy calculation times
Robotic-assisted spine surgery today is pretty much a flawless procedure compared to the early days.
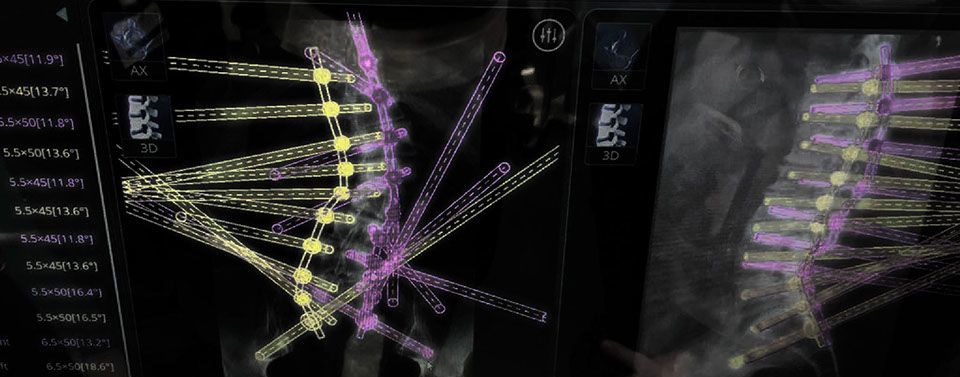
Software crashes and lengthy calculation times no longer exist. The advanced technology allows the surgeon not only a significant improvement in 3D visualization, but also in dexterity and coordination, increased precision in pedicle screw placement, as well as a reduction in fatigue during long operations.
For the patient, it offers a smaller incision, reduction of post-operative pain, minimal muscle retraction, and therefore faster recovery.
Robots tend to be especially useful for surgeries of patients with severe deformity, and for minimally invasive and revision surgeries in which anatomical landmarks are obscured, who have a high body mass index, or poor bone quality. The 3D planning software allows surgeons to pre-plan the procedure better and perform not only a more accurate, but also a more reproducible outcome.






 1 - 7<>
1 - 7<>
Robotic-assisted procedures are only as good as the surgeon performing them
One of the main challenges of robotic-assisted spinal surgery though is its technological complexity. Poor outcomes in surgery may occur if the technology is relied upon blindly. Robots have been developed to assist the surgeon, and not to replace him or her. Consequently, robotic technology can never make an incompetent surgeon good, but only help an experienced surgeon to become even better.
Anatomical knowledge and surgical experience are still key for good performance. Any surgeon operating with robotic assistance should also be able to operate the patient under ‘standard’ fluoroscopy- guidance case of any technical errors, just like a pilot needs to be able to fly his plane without auto pilot.
Translating robotic-assisted spine surgery into mainstream
Robotic system technology is a flourishing field these days. Traditional medical device manufacturers have teamed up with robotic companies. Technological advancements as well as the feedback from surgeons may lead to the development of very different robotic devices in the future, which will support the surgeon to perform even better.
Essentially, robotic-assisted surgery should be able to unite and advance both MIS and spine navigation techniques in such a way that it helps surgeons to perform complicated procedures in areas of the body that would normally be nearly inaccessible to human hands with greater agility, and way beyond what is currently possible.
Today's generation of robots in spine surgery work around a so-called "no-fly" zone – they get extremely close to the skin, but never touch the patient. The robot arm is guided straight down. In the not so far future, the surgeon could potentially be able to do things "around corners" with robotic guidance or have the robot drilling into the spine rather than doing it him- or herself.
There are more strings attached to these new technologies though. It's by far more than just the operating procedures that will need to be adapted.
There will also be changes and adaptions needed to the operating room workflow, the OR table itself, or even make an OR theatre more well adapted to CAN (Computer Assisted Navigation) procedures. Studies are needed to substantiate that the significant equipment costs, including the maintenance, software updates and technical support, will result in major benefits for the patients that will justify the expenses, as well as decrease the OR time.
It remains to be seen how robotic-assisted spine surgery will translate into mainstream spine surgery. Currently, the usage is limited in both procedure as well as the area of the spine where robotic-assisted surgery has been approved by the FDA (US). In order to gain acceptance amongst the worldwide spine surgeon community, robots must not only allow them to improve the procedures that they currently perform, but in order to truly revolutionize the field they must fundamentally improve how spine care is managed and how patients are approached.
00:00
00:00
More reproducible outcomes and better resource planning
It is obvious that great opportunities lie in robotic-assisted spine surgery that could help improve the outcomes significantly and make surgery safer for patients. But it's not only that. Robots could also help hospitals to significantly improve the supply chain management system and the workflow in the “OR of the future”, as instruments and pedicle screws could be ordered in advance according to the exact needs for the respective operation.
Just as in the airline industry, where planes are scheduled to depart from the gates right on the minute and the supply chain management for airplane maintenance is far advanced, robots in could better analyze how much time a surgery will take and plan the caseload more precisely and pre-order the exact equipment without redundancy.
As a result, surgeons will be able to be more efficient in fitting patients and hospitals in allocating their human resources better.
Robotics: Making the best surgeon
even better

Dr Kornelis Poelstra, MD
Dr Kornelis Poelstra is one of the world's most experienced experts in robotic assisted spinal surgery. In this exclusive interview he explains the enormous potential of robots to improve patient outcomes, run more efficient ORs and help even the most experienced surgeons to always bring their ‘A game’
How did you first become interested in the spine, and what caused your interest in robots?
I actually worked in car detailing and as a basic mechanic at Ford when I was 14 and subsequently Volvo until I was 23. I enjoyed engineering and working with my hands so when I started medical school I knew I wanted to specialize in orthopaedics.
A Nuffic (Dutch organization for internationalization in education) grant brought me to the US, where I completed my PhD in Biomedical Engineering and began a residency at the University of Virginia. It’s a powerhouse for Orthopaedics and Spine/Neurosurgery, which is how my interest in spine began. The residency was fantastic; spine was just for me. I was offered an Ortho-Neuro Fellowship at Thomas Jefferson with great mentors and after completion, I became assistant professor at the University of Maryland/Shock Trauma. I spent four years in Baltimore doing spine deformity and trauma, where I learned to do big surgeries and do them well.
My interest in robotics really goes back to my fascination with mechanics, but it was also a solution to two common problems we faced when doing complex reconstructions. Firstly, it seemed superfluous to have to expose everything, particularly when you have a really sick trauma patient. These patients come in as sick as can be, with multisystem organ failure and then on top an unstable spine – they’re too sick for an open spine operation. However if you can operate in the first 24 hours after a trauma with minimally invasive surgery, by just stabilising the patient, they do a lot better. I saw there were huge advantages, but the next challenge was fluoro-radiation with ‘conventional MIS’.
Even though we were pretty fast, a 10 level spine reconstruction took about four minutes of fluoroscopy. Navigation could only do so much with these patients, as any change in alignment of the spine made the registration back then very difficult. I thought, there must be a better way, and the answer was robotics.
I thought to myself that just like everywhere else, everything will at least partially become automated, even in medicine. I decided to stop saying ‘I’m a really good surgeon; I can do this without robotic devices’, because robots, like everywhere else in society, are here to stay. I want to be one of the first surgeons adopting this new technology while still in its infancy, so that I’ll be ready when the real machines are coming. I am going to be better prepared and I will know the nuances of robotic spine surgery better, I could teach more people about it and I could essentially serve my patients much better.
What technology are you using and how has it evolved since you started working with it?
I’ve been interested in Mazor systems since about 2008, when their first robotic system (Mazor Renaissance) became available. Because I was such a heavy user of their system since 2014, Mazor approached me and introduced me to the earliest Mazor X, and I've been collaborating very closely with them in the development. I’ve done about 200 Mazor X cases now, more than anyone else in the world. Early on, the systems couldn’t keep up with the huge amount of calculations; we had crashes, power outages, smoke coming from the machine, robot arms just stopping…. Luckily nobody ever got hurt. The ability to hang in there and see the value is what set us apart. Now the technology is so smooth and cases so quick that it’s a whole different philosophy. The future robot arms will be so stable that we can start thinking about doing decompression with them rather than just trajectory guidance, which is what it mostly is today.
What percentage of your procedures is robotic-assisted?
I've done about 400 robotic-assisted surgeries in total so far. I do pretty much all screw placements with the robot.
We’ve put in more than 3,000 screws and had zero failures. I do evidence-based surgery, and we’ve actually shown that the risk of running into any kind of complication is reduced three fold compared to minimally invasive cases using “freehand MIS” without the robot, and re-operation rates are also three- to four fold less.
Additionally, my readmission rates for these types of cases became significantly reduced. We simply are better prepared when we go into the OR due to the planning stage for the Mazor system. Once I have planned my case, I can execute it in a flawless fashion.
I am more relaxed in the OR because the robot will go exactly where I planned it, and it is just as easy to place a screw through a 2mm pedicle as it is to instrument a 10mm pedicle.
How important is surgical experience for doing robotic-assisted spine surgery?
I believe you need to be able to do a good technical surgery first to know what the anatomy looks and feels like, because then you’re going to be much better at appreciating the nuances of robotics. It’s a concern that some surgeons are emerging from training programmes having only experienced “MIS” via navigation and robotics. I think there should be a requirement to have done, say, 100 open cases and conventional freehand MIS cases so you can get yourself out of trouble if the technical tools fail you. On the flip side of that, for an experienced surgeon the move to robotics is very easy; the surgical team will need two or three cases to get used to the new tools and the surgeon will need about five cases to learn the nuances and a further 10-15 or so to fully appreciate the dos and don’ts. After about 20 procedures you really have it and can focus on honing your skills.
How do you believe robotics will change
spine care?
It’s a tremendous challenge as the early adoption of the technology comes with a cost, but you have to seriously look at the evidence of reduced complications and readmissions. It’s a test of humility to recognise that you might not be at your best after 12 hours surgery or a fight with your staff. We’re all human and we can’t be on our “A-game” at all times, so we should look for tools that will make us better. The ‘secret sauce’ is coming to the playground as you realize you will be a better prepared surgeon, and therefore more able to focus on the medical aspects of the case, and maybe be a better champion in the OR for your team. As surgeons, we are bred to be number one at what we do, and the challenge is to become humble and realize that there are highly advanced tools that actually make you better if you are willing to go through the learning curve.
In today’s world of Big Data, how does robotics help to capture statistics and ensure reproducibility of the outcomes?
Initially the robots were true trajectory guidance tools. Today's robotic systems go way beyond that. They are used as a data hub capturing and reporting everything we do. Robots have the potential to drive efficiencies and manage inventory better.
In the future, say I put in 10 screws over 5 levels during a surgery: imagine if the robot simply brings me the exact 10 screws and corresponding screwdrivers, instead of opening several trays of sterilized equipment at $100 each that have been shipped cross-country each time like we do today. Due to the pre-operation planning, the robot will be able to know and order everything that I will need for my operation. Having the exact equipment there without excess and make all of it disposable afterwards is so much more efficient and cost effective. The potential is enormous.
What are the characteristics of your ideal
future robot?
No matter all the advances, the number one thing is patient safety. The FDA doesn’t allow a robot to drill itself currently but in an ideal scenario I’d have the ability to touch the screen with my finger and have the robot drill- or decompress the spine where needed. Regulation-wise, we need to move forward safely and cautiously, with experienced surgeons working alongside industry and regulatory bodies.
Where do you believe the field of robotic surgery
is headed in the short and longer term?
I hope we’ll have two or three more systems hit the market soon because competition in this field is a good thing. Then, I think we’ll see much greater adoption of the technology to make it more mainstream than navigation ever was. I think that will happen within two years, and by five years, we will see the robot starting to do ‘active things’ for us like osteotomies or discectomies for interbody reconstructions.
The next generation of tools will be safer and faster than working by hand, and the surgeon’s role is fine-tuning and checking it. Open exposure of the spine will still be necessary in some procedures of course.
Lastly, robots can only become great if they can make a really good, fast surgeon even better. And the way the technology is going… This is very much worth pursuing!
_________
Biography:
Kornelis Poelstra MD PhD is Orthopaedic- and Neurological Spine Surgeon. He is the President of the The Spine Institute on the Emerald Coast in Destin, Florida (USA) and the Chairman of the Department of Surgery of the Sacred Heart Hospital on the Emerald Coast.
Newsletter 11
May 2017
