Brave new world: a 3D future?
Nearly two decades have passed since 3D printing first crept into the manufacturing sector, yet despite considerable media attention, its biomedical applications are still little understood. So is 3D printing truly a brave new world for personalized medicine, or an unrealistic dream?

"The combination of 3D modelling and biomedical tissue engineering is the future for surgery."
Read the interview with Risto Kontio
As with any technological breakthrough, advances in 3D printing have attracted countless media headlines breathlessly proclaiming a ‘world first’. These range from unsettling homespun innovations, such as the student who claimed to have created the world’s first 3D printed revolver in November 20151, to the pioneering, like the January 2016 tale of a Northern Ireland toddler who became the first in the world to receive an adult kidney transplant with the help of 3D modelling and manufacturing2.
Recent months have also brought a number of prospective breakthroughs in 3D printing for spinal surgery. In July 2015, a German medical team successfully fitted the first 3D-printed titanium fusion implant to a patient with a degenerative cervical spine condition3. Professor Uwe Spetzger, a neurosurgery specialist at the Klinikum Karlsruhe in the state of Baden-Württemberg, planned and executed the surgery in collaboration with 3D-printed implant company EIT and its partner 3D Systems.
Additive manufacturing
3D printing – or additive manufacturing as it’s more formally known – is a layering process that enables the creation of incredibly complex and delicate structures. While early additive technologies utilised ink and plastic, a sophisticated new method of Selective Laser Sintering (SLS) uses powdered material to create highly intricate models in metals, plastics and ceramics. In Prof Spetzger’s surgery, SLS facilitated the creation of a cellular titanium cage which mimics the trabecular bone structure, allowing natural bone to regenerate without the need for a bone graft. In place of a standardized model, the patient received a highly bespoke implant, reducing the risks of implant migration, subsidence or delayed fusion. The success of the procedure led Prof Spetzger to declare: “The future of patient-individualized spinal implants has begun.”
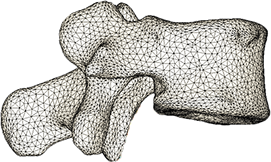
Indeed, later that year Australian neurosurgeon Ralph Mobbs removed cancerous vertebrae from a patient with chordoma – a rare form of cancer that occurs in the bones of the skull and spine – and replaced these with 3D printed vertebrae4. Because of the position and function of the vertebrae, individualization was crucial to the success of the procedure, and 3D printing firm Anatomics built exact anatomical models of the patient’s skull for the surgeon to practise on, then printed new titanium vertebrae for a precise fit.
Growth predictions
Yet exciting as the applications clearly are, how close are we to actually realising this vision of low cost, high efficiency, personalized biomedical technology? In a detailed report titled Medical Applications for 3D Printing: Current and Projected Uses, author C. Lee Ventola provides statistics that point to an astonishing growth sector5. Since the early 2000s, 3D printing in medicine has grown from relatively small-scale use for dental implants and prosthetics to a vast range of applications including tissue and organ fabrication, prosthetics, implants, anatomical modelling and pharmaceutical research concerning drug discovery delivery and dosage. 3D printing has created everything from bones and ears to blood vessels and organs.
According to Ventola’s research, in 2014 3D printing was a $700m industry, with medical applications accounting for only 1.6% of that value. In 10 years, the industry is projected to be worth at least ten times that, at $8.9bn. By 2024, projections suggest that the medical applications of 3D printing will account for around 21% of its market value, at $1.9bn. While Ventola cautions that the technology needs committed time and effort to mature and enter the mainstream market, he points out that we are an estimated 20 years away from the first printed human heart, while in future it may be possible to create a complete toolkit of organs and tissues from stem cells derived from a child’s baby teeth.
Problem solving
While 3D printing has in itself captured the popular imagination, it’s true potential is best understood as part of a wider suite of digital visualization tools. Writing in Live Science6, Scott Dunham of SmarTech Markets (an industry analysis and market forecasts company for the additive manufacturing industry) claims: “We recently produced a 10-year forecast for the field, and there is an unusually strong synergy among digital 3D design, medical imaging and 3D printing for medical applications. The three form a trifecta of medical problem-solving power, where physicians can use patient-specific data to capture, manipulate and ultimately apply physical solutions of all shapes and sizes through 3D printing. Without such technology, personalized medicine would be difficult, as patients will need unique parts that can be rapidly and simply manufactured.”
In practice, this means that medical teams will be able to build 3D models of their patients’ anatomy and use it to pre-plan and even practise their surgical technique, before manufacturing the necessary prosthetic or implant to precisely fit the model. Dunham points to the case of two-year-old Mina Khan, who suffered from a large hole in the ventricles of her heart. Her operating team at St Thomas Hospital in London used MRI and CT scans to develop a 3D model of her heart, which gave them an accurate understanding of the defect and the exact positioning of a custom GORE-TEX® patch7.
Then there’s the case of Zeesy Stern, a patient at NYU Medical Center who benefited from what her surgeon Dr Jamie Levine nicknamed ‘a jaw in a day’. The team used CAT-scan images to design a 3D model of Stern’s skull, which was then used to create a metal plate and plastic surgical guides indicating where to cut or drill. The new jaw was manufactured from bone in Stern’s leg, achieving a precise fit. The cutting guides were FedExed to the surgeons by manufacturers 3D systems, allowing doctors to work simultaneously. A procedure that previously took three operations over 18 months at a cost of $20–$30k was made better, quicker, simpler and cheaper.
The 3D model reduced the amount of “eye-balling”, said Dr Levine. In a conventional setting, the surgeon would be guided by scans but would ultimately have to open the patient up before deciding the best surgical approach, then use a scalpel and drill to customize the implant. 3D technologies removes some of that guess work and delivers individually tailored implants and prosthetics.
A paradigm shift?
Of course, another major benefit of 3D printing is cost. Because traditional manufacturing relies on the creation of unique molds and the operation of multiple expensive machines, the cost of complex medical implants and prosthetics is prohibitive, and the time to market high. By contrast, a single 3D printer is capable of producing any device, the only additional cost being that of materials. Since it does not rely on a complex production chain, 3D-printed materials also have the benefit of being quick to deliver, with some being fabricated within 24 hours. Finally, the industry is hailed by some as a democratizing source for medical research, because it allows researchers to share an exact replica of a medical model or device through downloadable .stl files available on open-source databases8. In response, the US National Institute for Health has established a 3D Print Exchange to maximize the opportunity.
The benefits are clear, but of course there are still some major barriers to overcome before the technology can be made widely available to healthcare professionals internationally. The first barrier is a practical one: that of cost and skillsets. Currently, the average medical grade 3D printer costs in excess of $200k, and medical professionals would need to dedicate considerable time to mastering the software before it could be adopted for the safe production of clinical models, tools or implants. Yet both working practices and industry manufacturers are finding innovative solutions. The price of printers is falling, with companies such as BioBots launching a $10k model available to scientific researchers for as little as $5k. Once the initial investment is made, the cost savings over time are potentially enormous. Meanwhile, some hospitals in New York are trialling in-house 3D printing centers where trained staff can lead production and pass on their expertise. “The main limitation of 3D printing is not functionality or cost but awareness of what can be done,” says Dr Oren Tepper, director of craniofacial surgery at Montefiore Medical Center in New York, who is pushing forward proposals for an on-site printing center.
Awareness is not the only problem – perception is another barrier that must be overcome before additive manufacturing enters the mainstream of medicine. In a section of Medical Applications for 3D Printing titled ‘Barriers and controversies’ Lee Ventola points out that developments such as gun printing have led to serious concerns around safety and responsibility, and highlight the need for tight regulation to prevent misuse of the technology, for example to create counterfeit devices and medications. Meanwhile, existing regulation over new drugs and technologies entering the market slows the pace of innovation, and some regulators such as the US FDA have created a working group to help realize the potential of this booming new industry.
While 3D technology is not without its challenges, it seems that these challenges are those commonly facing new and pioneering treatments, and will in time be overcome. Expert analysts such as Dunham predict that within a decade 3D models and custom guides will be standard procedure, while Dr Levine points out that in 1995, CAT scans were just as novel as 3D printers are now9. “3D technology,” says Levine, “is a paradigm shift in the way we do surgery.”
Dr Risto Kontio is currently Chair of Department of Oral and Maxillofacial Surgery at Helsinki University Hospital. He has been a chair of Research and Development Commission of AOCMF since 2011. He is also a secretary of the Board of Oro-Maxillo-Facial Surgeons / UEMS since 2013. His main research area is reconstructive surgery. He has written his thesis on orbital reconstructions.

Helsinki University Hospital was an early adopter of additive manufacturing, or 3D printing as it’s more commonly known. How is this technology used in the surgical setting?
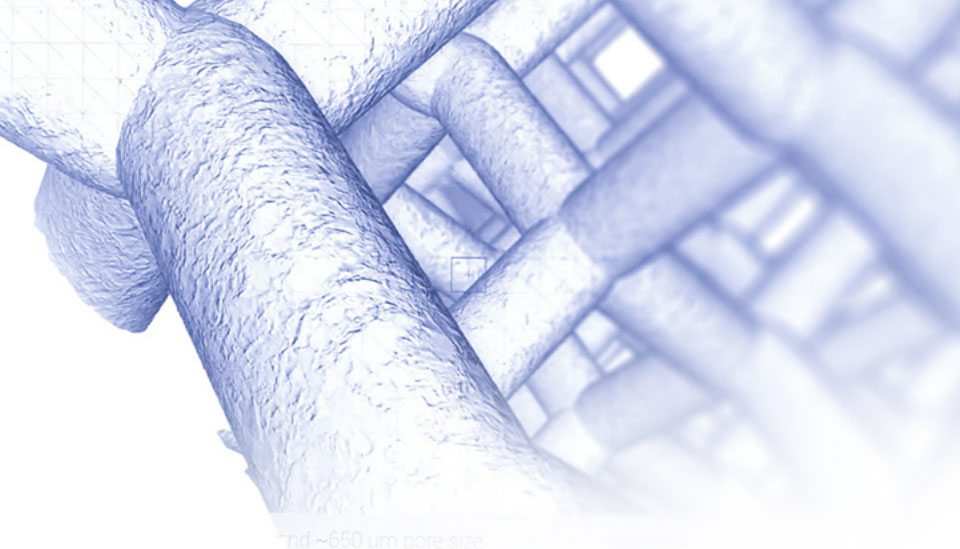
We use 3D printing all the time, within two main applications. On the commercial side, we have access to both sophisticated CAD software (Computer-Aided Design) and a 3D printer through a private Helsinki company. We use this to plan and simulate surgery and produce scaffolds, plates and surgical devices, all customized to the individual patient. These devices are mostly fabricated from sterilized titanium then used for fractures and reconstructive surgeries. The second application of 3D technology is through the hospital’s own printer, which we use to create accurate 3D models to guide surgeries. For example, we can use a CT scan (computed tomography) to create an exact image of a patient’s jawbone on screen, then convert DICOM data into an STL file and feed that data into a 3D printer. We then have a perfect, solid model that we can hold in our hands, rotate and cut to size. This second application is particularly useful to us as a teaching hospital, as it helps young surgeons to visualize the problem and procedure.
How is this planning and simulation executed during the actual surgery?
A surgeon would use navigation to execute the planned surgery, but we prefer to use guiding devices created on our 3D printer. It’s a small piece of sterilized plastic that acts as a template to ensure your cuts are in exactly the right location. We also print patient-specific plates, which save lots of time on bending, as they fit directly onto the bone. Instead of spending 30–40 minutes cutting and bending, the customized plate takes seconds to fit. This significantly reduces the length of the surgery.
How does this benefit impact on overall patient outcomes?
For the patient, the main advantage is the shorter surgery time. We know from general research and experience that the longer the operation, the higher the risk of complications. 3D technologies have significantly reduced both, and patients after major surgery now spend roughly one to two nights less in intensive care than previously.
For younger patients requiring reconstructive surgery – for example due to cancer in the facial area – patient-specific implants provide an alternative material to bone. While for adults we can harvest the patient’s own bone as microvascular flap, this isn’t possible for children, as it would upset their growth. Instead, we now have the option of 3D printing materials that mimic bone and using them for reconstructive surgeries until the patient reaches adulthood. Again, young patients also benefit greatly from the reduced surgery time.
Of course, yours is one of few hospitals utilizing this technology. What are the main barriers that prevent 3D printing from being more widely adopted?
Cost is the main limiting factor. A high-end 3D printer is still very expensive to buy, and then you have the additional costs of maintaining an engineering service to operate the printer and CAD technologies. The virtual planning, design software and simulation are all very complex, and while I expect it will become simpler in future, it’s not feasible for surgeons to train to use the technology. It will probably always require a close collaboration between medical doctors and engineers.
It was this kind of collaboration that first opened the door to 3D technology for us, some six or seven years ago. We were working with a technical university in Helsinki and this caught the attention of a private company, which invested in the hospital to develop its potential. Today there are only 10–15 hospitals in Europe using 3D technology at this level, so we’re very fortunate. When we first started creating patient-specific 3D implants the process took around 150 days from the initial x-ray to holding the implant in your hands. Today, it’s 24 hours.
Many of the design programs for 3D printing are available as free, open source files, creating both an opportunity for collaboration and a challenge for regulators. Do you think more regulation is needed to protect patients?
There are risks attached to any new technology or procedure, so perhaps greater regulation will be necessary but it’s hard to say right now. I think the main issue could be maintaining the quality of the materials. Titanium is very relatively expensive which could create a market for lower quality copies. It’s a situation that will need to be monitored over time.
There’s a lot of hype around 3D technology as the future of surgery – is that a realistic vision in your opinion?
Yes it is, but the second area I see as even more important in the years ahead is that of tissue engineering. There are incredibly sophisticated 3D printers now which can incorporate live cells into the printing material to create bone. This combination of 3D modelling and biomedical tissue engineering is the future for surgery. We’re in close collaboration with other institutes across Europe to explore this technology. Collaboration is very important as it gives provides greater volume and introduces new ideas and perspectives on how we can make the most of these innovations.
3D printing and tissue engineering: the future of surgery
Dr Risto Kontio, Senior Maxillofacial Surgeon and Chair of the Department of Oral and Maxillofacial Surgery at Helsinki University Hospital, shares his views on the potential of 3D printing
- http://3dprint.com/107062/worlds-1st-3d-printed-revolver/
- http://www.telegraph.co.uk/technology/2016/01/26/toddler-gets-world-first-adult-kidney-transplant-using-3d-printi/
- http://www.spinalsurgerynews.com/2015/07/3d-cervical-titanium-implant/11620
- http://www.wired.co.uk/news/archive/2016-02/26/3d-printed-vertebrae
- C Lee Ventola, 2014. Medical Applications for 3D Printing: Current and Projected Uses http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4189697/#b3-ptj4910704
- http://www.livescience.com/49913-3d-printing-revolutionizing-health-care.html
- http://3dprintingindustry.com/2015/02/08/another-heart-mended-3d-printed-surgical-model/
- Gross BC, Erkal JL, Lockwood SY, et al. Evaluation of 3D printing and its potential impact on biotechnology and the chemical sciences. http://www.ncbi.nlm.nih.gov/pubmed/24432804
- http://www.plasticsnews.com/article/20160111/NEWS/160119985/3-d-printing-and-surgery-a-paradigm-shift
Newsletter 8 September 2016